What is Medical Device Clinical Evaluation?
Medical device clinical evaluation is a systematic process that assesses their safety and performance using clinical data. This process is crucial for confirming whether a device complies with regulatory requirements and is safe for patient use. The evaluation involves reviewing clinical trials, analyzing real-world evidence, and studying scientific literature. Its primary aim is to confirm that the device’s benefits outweigh any possible risks.
Medical Device Clinical Evaluation - Regulatory Requirements
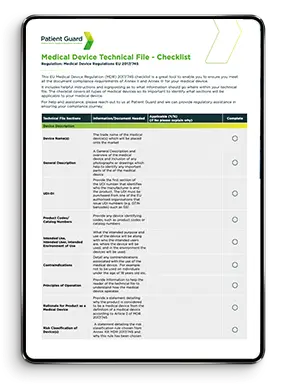
Before a manufacturer can place their medical devices on the EU or UK market, they must demonstrate compliance with the relevant medical device regulations. For CE marking, manufacturers must meet the requirements of the Medical Device Regulation (EU) 2017/745. For UKCA marking, compliance with the UK Medical Device Regulations 2002 (as amended) is required.
Specific Requirements
These regulations include specific requirements for conducting a clinical evaluation. In the EU MDR 2017/745, these requirements are detailed in Annex XIV. For the UK MDR 2002, clinical evaluation is outlined in Annex X of the Medical Device Directive 93/42/EEC.
Medical Device Clinical Evaluation Guidance Documents
The clinical evaluation of medical devices, as required by medical device regulations, has often caused confusion for manufacturers. Many are unclear about what is expected from a regulatory standpoint. To address this, regulatory bodies have issued guidance documents. These documents explain how they interpret the requirements for clinical evaluation and how manufacturers should present this information. This ensures that medical devices meet compliance standards.
Regulatory Framework
The primary guidance document for conducting clinical evaluations is still MEDDEV 2.7/1 Revision 4. While the MDCG (Medical Device Coordination Group) documents related to EU Regulation 2017/745 provide guidelines on the topic, they do not offer specific instructions for performing a clinical evaluation. Instead, they focus on broader guidance around the subject.
Clinical Evaluation Plan
The starting point for a clinical evaluation is developing a Clinical Evaluation Plan (CEP). The CEP outlines how the manufacturer will conduct the clinical evaluation. It includes details on the approach to scientific literature searches, the methodology, and the research methods used. This ensures that the clinical data collected adheres to a valid scientific process.

Scope
The plan defines the scope of the clinical evaluation and specifies the types of data that will be used. It also identifies the relevant regulatory requirements applicable to the device, ensuring its performance and safety are thoroughly demonstrated.
What Data is used in Medical Device Clinical Evaluation?
To demonstrate that a medical device is safe and performs as intended for its clinical use, presenting the correct data is crucial. Manufacturers must provide pre-clinical data, clinical data, and risk management data to meet regulatory requirements.
Pre-Clinical Data
Pre-clinical data includes the medical device’s design history, manufacturing information, product details, packaging, handling, transport, storage verification, and usability data. This data should align with harmonized or consensus standards where applicable. In cases where no standards exist, manufacturers must demonstrate robust verification and validation methods to confirm that the device meets its intended specification inputs.
Verification & Validation data
Verification and validation activities must confirm that design and manufacturing outputs meet the specified inputs. They should demonstrate that the finished medical device functions as intended and has been designed and manufactured to address all known and foreseeable risks identified through risk management processes. These risks must be reduced as much as possible, following ISO 14971, the standard for medical device risk management.
All Aspects of the device
This approach applies to all relevant aspects of the device, including packaging, sterility, software, and electronics, using consensus standards where applicable. The data should incorporate a statistical approach to sample sizes to ensure the results are repeatable and reliably demonstrate the device’s performance and safety.
Biological Evaluation
If a medical device has direct or indirect contact with the body, such as a tube delivering a substance, it must undergo biological evaluation. This evaluation should be conducted on the finished, manufactured device. As a critical part of pre-clinical data, biological evaluation ensures the device is toxicologically assessed. It must be completed before any human trials or studies to confirm the device’s safety for use.
Clinical Data

Clinical Trials/Clinical Studies
For novel medical devices or legacy devices being used for a new intended purpose with no clinical history, clinical trials are typically required. These trials generate supporting evidence to demonstrate that the intended use aligns with the “state of the art.”
Published Clinical data
Published clinical data on safety, performance, and clinical background should be sourced using established research methods. Reputable sources like PUBMED, the Cochrane Library, and other peer-reviewed literature databases are essential for identifying relevant data.
Un-published Clinical data
The medical device manufacturer may use data from clinical trials on the device itself that have not been published as evidence that the device is safe and effective.
Risk Management Data
The clinical evaluation should incorporate data from the manufacturer’s risk management activities, which assess all known and foreseeable risks associated with the medical device. These activities must comply with the requirements of ISO 14971, the standard for medical device risk management.
Who should perform Medical Device Clinical Evaluation?
Clinical evaluation should involve a multidisciplinary team. This team should include clinical experts familiar with the device’s intended use, medical device specialists with technical knowledge, and regulatory experts who understand the evidence requirements and how to present them effectively.

Clinical Experts
The clinical evaluation team should include experts with experience and knowledge specific to the clinical intended use and clinical background.
Medical Device Experts
The clinical evaluation team should include experts with knowledge about the medical device itself, such as the design and development team, quality engineers.
Regulatory Experts
The team should also include expertise from regulatory professionals who can advise on the regulatory requirements, standards, guidance documents, clinical /medical writing etc.
Clinical Evaluation Report
After all data has been assessed and critically reviewed, it should be compiled into a Clinical Evaluation Report (CER). This report must provide a thorough analysis of the pre-clinical and clinical data, demonstrating that the benefits of using the medical device outweigh the associated risks, considering its intended use.
EU Guidance
The Clinical Evaluation Report (CER) should follow regulatory guidance documents, such as MEDDEV 2.7/1 Revision 4 and relevant MDCG documents. Adhering to these guidelines ensures that clinical evaluation data and conclusions are presented consistently for assessment by Notified Bodies or Regulatory Authorities.
Notified Bodies
It is crucial to note that a Notified Body may involve multiple team members in evaluating your medical device technical documentation. The person reviewing the Clinical Evaluation Report (CER) might not be the same individual assessing other parts of the technical file. Therefore, the CER should include complete summary data rather than referencing other sections of the technical file to ensure clarity and consistency.
Post Market Clinical Evaluation
Clinical evaluation is an ongoing process, not a one-time event. The initial evaluation supports obtaining CE marking or UKCA marking for the medical device. After the device is on the market, clinical evaluations must be repeated regularly, with the frequency determined by the device’s risk level.
Clinical Evaluation Updates
A two-year timeframe is commonly used as a benchmark for updating clinical evaluation reports. The updated report should assess any new clinical data generated since the previous evaluation. It should also include information from Post-Market Surveillance (PMS) activities and any Post-Market Clinical Follow-up (PMCF) data collected.
Post Market Surveillance (PMS)
Manufacturers must generate a PMS Report or PSUR annually, depending on the medical device’s classification. Class I device manufacturers prepare PMS Reports, while manufacturers of Class IIa and higher devices must create PSURs. This information should be summarized in the updated Clinical Evaluation Report.
Post Market Clinical Follow-up (PMCF)
Medical device manufacturers must conduct Post-Market Clinical Follow-up (PMCF) alongside Post-Market Surveillance (PMS) activities. PMCF gathers real-world clinical data from device users. Manufacturers should prepare annual PMCF reports analyzing this data and how the devices are used in practice. The findings from these reports should be summarized in the updated Clinical Evaluation Reports.
Summary
The clinical evaluation of medical devices is vital for assessing their safety, performance, and effectiveness. This process involves analysing clinical data from sources such as clinical trials, real-world use, and scientific literature. It plays a key role in regulatory approval and post-market surveillance, ensuring the device meets the required standards for safe patient use. Clinical evaluation includes a thorough review of pre-market and post-market data to identify risks, benefits, and areas for improvement. Its primary goal is to demonstrate a favourable risk-benefit profile, ensuring patient safety and effectively addressing medical needs.
FAQ's
Clinical evaluation is a systematic process of assessing and analyzing clinical data to verify the safety and performance of a medical device. It is a regulatory requirement under the EU Medical Device Regulation (MDR) 2017/745, ensuring that the device meets its intended purpose and is safe for use in patients.
Why it’s important:
Clinical evaluation provides evidence that a medical device delivers the intended benefits while minimizing risks. It forms the foundation for regulatory approvals and post-market surveillance.
The clinical evaluation process under the EU MDR consists of the following steps:
- Scoping and Planning: Define the device’s intended purpose, clinical claims, and evaluation scope.
- Identification of Data: Gather clinical data from literature, clinical investigations, or post-market data.
- Appraisal of Data: Assess the relevance, quality, and adequacy of the collected data.
- Analysis of Data: Evaluate whether the data supports the device’s safety and performance.
- Clinical Evaluation Report (CER): Document findings and conclusions in a comprehensive report.
Pro tip for manufacturers: A well-structured CER can significantly streamline the regulatory submission process.
A Clinical Evaluation Report (CER) is a document summarizing the clinical evaluation process, findings, and conclusions. It demonstrates the device’s safety and performance based on clinical evidence.
Why it matters:
Regulators and notified bodies rely on the CER to assess whether a device meets EU MDR requirements. An inadequate CER can lead to delays in market access or non-compliance issues.
Post-market clinical follow-up (PMCF) is a continuous process of collecting and evaluating clinical data after the device is placed on the market. It ensures that the clinical evaluation remains up-to-date throughout the device lifecycle.
Key goals of PMCF:
- Detect long-term safety or performance issues.
- Validate the continued benefit-risk profile of the device.
- Address gaps in pre-market clinical data.
Tip for manufacturers: PMCF activities should be integrated into your overall post-market surveillance plan.
Absolutely! Patient Guard specializes in helping medical device manufacturers navigate clinical evaluation requirements under the EU MDR. Our services include:
- Developing compliant clinical evaluation plans and reports.
- Reviewing and appraising clinical data.
- Assisting with PMCF planning and implementation.
Why choose us: With experience in over 500 successful client projects, we provide tailored solutions to ensure your device’s regulatory success.