Introduction
In this blog, we’ll break down the key steps in the EU medical device regulatory roadmap and provide guidance to help manufacturers navigate the process efficiently and effectively.
Why Understanding the EU Regulatory Roadmap Matters
The EU MDR replaced the Medical Device Directive (MDD) in May 2021, introducing stricter requirements for safety, performance, and post-market surveillance. Failing to comply with the MDR can result in product delays, costly redesigns, or even market withdrawal.
Whether you’re developing a new product or updating an existing one, understanding the regulatory roadmap is essential for:
Ensuring product safety and compliance
Achieving CE marking
Gaining access to the EU market
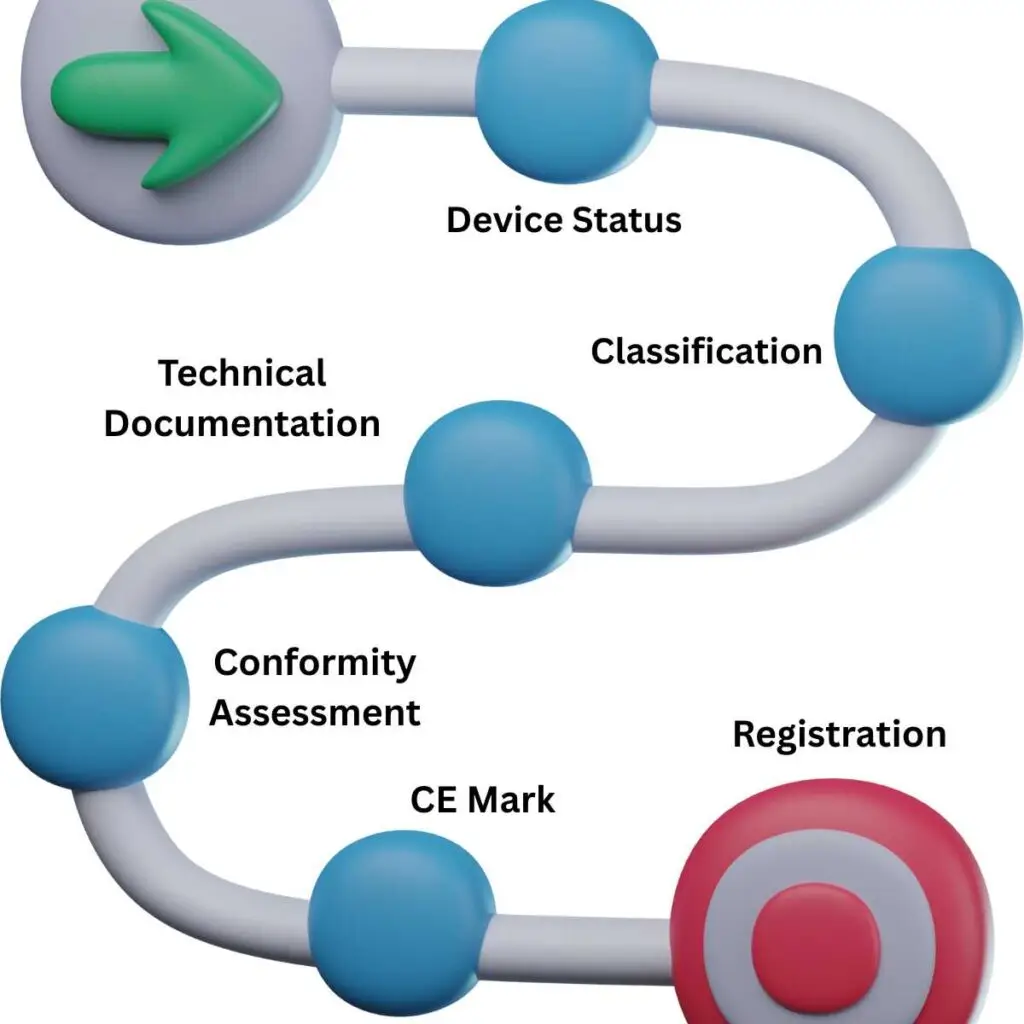
Step 1: Determine if Your Product is a Medical Device
Start by identifying whether your product meets the definition of a medical device under the MDR (Article 2). This step is critical, especially for borderline products or software.
Tip: Patient Guard offers tools and expert guidance to help you determine if your product qualifies as a medical device.
Step 2: Classify Your Device Under MDR Rules
Under MDR Annex VIII, devices are classified into four categories: Class I, IIa, IIb, and III, based on risk. The classification determines the conformity assessment route and the level of involvement from a Notified Body.
Key Factors Affecting Classification:
Intended purpose
Duration of use
Invasiveness
Whether the device is active or non-active
Step 3: Choose the Appropriate Conformity Assessment Procedure
Depending on your device’s classification, you must follow a specific conformity assessment route. For higher-risk devices (Class IIa and above), this includes assessment by a Notified Body.
Common procedures include:
Step 4: Prepare Technical Documentation
The technical file must demonstrate compliance with General Safety and Performance Requirements (GSPRs) in Annex I of the MDR. It should include:
Step 5: Implement a Quality Management System (QMS)
For most devices, especially Class IIa and above, a certified QMS aligned with ISO 13485 is mandatory. The QMS should cover all stages of the product lifecycle, including design, manufacturing, distribution, and post-market activities.
Step 6: Conduct Clinical Evaluation
Clinical evaluation is essential to demonstrate the safety and performance of your device. It must be proportional to the device’s risk and based on:
Clinical data from the device or equivalent devices
Literature reviews
Clinical investigations (if necessary)
Step 7: Apply for CE Marking
Once the conformity assessment is complete and you’ve received the necessary certification from a Notified Body (if applicable), you can draw up your Declaration of Conformity and affix the CE mark to your device.
This mark confirms your product meets EU safety, health, and environmental protection requirements and can be legally marketed across the EU.
Step 8: Register Your Device and Manufacturer Details
Under the MDR, manufacturers must register their details and devices in the EUDAMED database. This includes:
Manufacturer information
Device UDI (Unique Device Identifier)
Certificates and regulatory status
Step 9: Post-Market Surveillance and Vigilance
Regulatory compliance doesn’t end after CE marking. You must monitor your device’s performance throughout its lifecycle. This includes:
Final Thoughts: Why Work with a Regulatory Partner?
The EU medical device regulatory roadmap can be overwhelming—especially for start-ups and SMEs. Partnering with an experienced consultancy like Patient Guard helps streamline your compliance journey.
We support you through every stage of the process, from product classification and technical documentation to Notified Body engagement and post-market support.
Frequently Asked Questions (FAQs)
The MDR significantly increases regulatory requirements compared to the MDD. Key changes include expanded scope (covering more devices and software), stricter clinical evidence requirements, enhanced post-market surveillance, and more rigorous Notified Body oversight.
The timeline varies depending on device classification, technical readiness, and Notified Body availability. For Class I devices, it could take a few months. For Class IIa, IIb, or III devices requiring Notified Body involvement, the process can take 12–24 months.
No. Only higher-risk devices (Class IIa, IIb, and III) require Notified Body involvement. Class I devices without a measuring function or sterility component can be self-certified by the manufacturer.
While not explicitly required, having an ISO 13485-certified QMS is strongly recommended and often expected by Notified Bodies. For most device classes, a compliant QMS is essential for CE marking.
Resources
How 5G Connectivity is Revolutionizing the Medical Device Industry
The Internet of Medical Things (IoMT): Connecting Wearable Devices for Remote Patient Monitoring
Storage, Handling and Transport Validation of Medical Devices
Streamline EU MDR Compliance with Patient Guard’s Medical Device Software Tools