What is MDR?
The Medical Device Regulation (EU 2017/745) came into full effect on May 26, 2021, replacing the previous Medical Device Directive (MDD) and Active Implantable Medical Device Directive (AIMDD). The MDR was introduced to address gaps and inconsistencies in the previous directives and to enhance the safety and performance of medical devices throughout their lifecycle. The regulation is legally binding and must be adhered to by all economic operators, including manufacturers, importers, and distributors within the EU.
MDR is considered a significant regulatory shift as it introduces stricter requirements for clinical evaluation, post-market surveillance, and technical documentation. Unlike the previous directives, MDR applies not only to traditional medical devices but also to products without a medical purpose, such as cosmetic contact lenses and dermal fillers. This broadened scope requires manufacturers to assess their entire product portfolio to determine whether products that were previously unregulated now fall under MDR.
Why Was MDR Implemented?
MDR was implemented to address several key challenges that were prevalent under the previous MDD and AIMDD frameworks:
Strengthened Device Classification:
Ensuring that devices are classified based on risk, duration of use, and invasiveness. This new classification system reflects a more comprehensive risk-based approach, requiring manufacturers to demonstrate compliance with more stringent standards, especially for higher-risk devices.
Enhanced Traceability:
Introducing the Unique Device Identification (UDI) system for better device tracking and identification. The UDI system allows regulators, healthcare professionals, and patients to trace a device throughout its lifecycle, promoting transparency and safety.
Clinical Evidence Requirements:
Requiring manufacturers to provide robust clinical data to demonstrate device safety and performance. Under MDR, clinical evaluation is a continuous process that must be maintained throughout the device’s lifecycle.
Increased Transparency:
Establishing the European Database on Medical Devices (EUDAMED) to provide public access to device information, clinical data, and regulatory certificates. EUDAMED consists of six interconnected modules that include device registration, notified bodies, clinical investigations, and post-market surveillance.
Key Players in MDR
To comply with MDR, several actors within the supply chain must understand their roles and responsibilities:
Manufacturers
Responsible for ensuring devices meet MDR requirements and for maintaining technical documentation. They must also implement a Quality Management System (QMS) in line with ISO 13485 and maintain post-market surveillance systems.
Authorised Representatives:
Appointed by non-EU manufacturers to represent them in the EU market. Authorised Representatives act as a liaison between the manufacturer and regulatory authorities, ensuring that the technical documentation and conformity assessments are up to date.
Importers and Distributors:
Responsible for verifying that devices are MDR-compliant before placing them on the EU market. Importers must confirm that the device is CE marked, has a valid Declaration of Conformity, and is correctly labelled with the UDI.
Device Classification under MDR
Devices under MDR are classified into four risk categories: Class I, Class IIa, Class IIb, and Class III. The classification is based on factors such as the duration of contact with the body, the degree of invasiveness, and the device’s intended purpose. Unlike the previous MDD classification rules, MDR introduces new rules for software, reusable surgical instruments, and nanomaterials, reflecting emerging technologies and risk profiles.
Class I:
Low-risk devices such as bandages and non-invasive medical instruments. Some Class I devices now require involvement of a Notified Body if they are sterile, reusable surgical instruments, or have a measuring function.
Class IIa:
Medium-risk devices such as administration sets.
Class IIb
Higher-risk devices such as ventilators and bone fixation plates. These devices typically require rigorous clinical data and a notified body review.
Class III:
High-risk devices such as implantable pacemakers and heart valves. Class III devices require the most stringent conformity assessment procedures, including clinical investigations and post-market follow-up.
Steps to MDR Compliance
Achieving MDR compliance requires a structured approach involving multiple stages of regulatory assessments and documentation. Here are the key steps to MDR compliance:
1. Determine Device Classification
Identify the appropriate classification based on Annex VIII of MDR. Misclassification can lead to regulatory delays and potential product recalls.
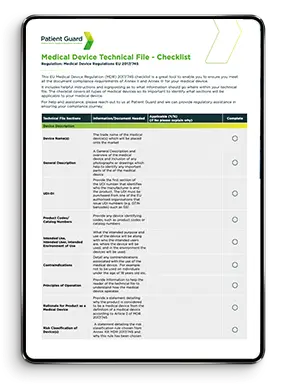
2. Compile Technical Documentation:
Prepare documentation that provides evidence of device compliance, including clinical data, risk management reports, biocompatibility testing, and electrical safety assessments.
3. Conduct Clinical Evaluation:
Demonstrate device safety and performance through clinical evidence. Clinical evaluation reports (CERs) must be prepared and continuously updated throughout the device’s lifecycle.
4. Implement a Quality Management System (QMS):
Develop a QMS that complies with ISO 13485 or similar standards, ensuring that manufacturing processes, risk management, and post-market surveillance activities are aligned with MDR requirements.
5. Appoint an Authorised Representative:
For non-EU manufacturers, appoint an EU Authorised Representative to handle regulatory obligations, including maintaining technical documentation and communicating with regulatory authorities.
6. Register with EUDAMED:
Ensure device information is registered in the EUDAMED database. EUDAMED registration is mandatory for all medical devices and provides greater transparency across the EU market.
7. Conduct Post-Market Surveillance:
Implement a post-market surveillance system to monitor device performance, collect clinical data, and address safety concerns. Vigilance reporting and periodic safety update reports (PSURs) are crucial components of ongoing compliance.

Common MDR Challenges and How to Overcome Them
Compliance with MDR can be complex, especially for companies that previously operated under MDD or AIMDD. Common challenges include:
Interpreting New Classification Rules:
The new classification rules can lead to higher-risk classifications, requiring more rigorous clinical evaluation and technical documentation.
Managing Clinical Data Requirements:
MDR demands comprehensive clinical evidence, even for legacy devices that were previously on the market. Manufacturers must establish a clinical evaluation plan and gather post-market clinical follow-up data.
Navigating EUDAMED Registration:
Understanding the EUDAMED database structure and ensuring accurate data entry can be challenging, particularly for small and medium-sized enterprises (SMEs).
Establishing a QMS:
Implementing a compliant QMS involves more than just documentation; it requires ongoing process management, internal audits, and risk mitigation strategies.
Frequently Asked Questions (FAQs)
The MDR transition period allowed for devices certified under the MDD or AIMDD to remain on the market until May 26, 2024, provided they meet specific conditions. However, after this date, all devices must comply with MDR requirements, including updated technical documentation, clinical evidence, and post-market surveillance. There is an extension for Class III medical devices until December 2027, for Class IIb and Class IIa medical devices there is an extension until December 2028, and for medical devices that did not require a Notified Body under MDD or AIMDD but require one under MDR there is an extension until December 2028.
As of now, EUDAMED is not yet fully operational, but several modules are available for voluntary use, including the actor registration module and the UDI/Device Registration module. Full implementation is expected to enhance transparency and device traceability across the EU market.
Under MDR, software that performs a medical function, such as monitoring or diagnosing a medical condition, is considered a medical device and must be classified according to its intended purpose and risk. The regulation provides specific classification rules for SaMD based on risk level and potential harm to patients.
Devices that do not meet MDR requirements by the applicable deadlines cannot be legally placed on the EU market. Non-compliance can result in product recalls, fines, and potential legal actions against manufacturers or importers.
How Patient Guard Can Help
Navigating the complexities of the EU MDR can be challenging, especially for companies unfamiliar with the stringent regulatory landscape. Patient Guard offers tailored consulting services to assist manufacturers, importers, and authorised representatives in achieving and maintaining MDR compliance. Our services include:
- Device Classification and Risk Assessment: We help manufacturers accurately classify their devices under MDR.
- Technical Documentation Review and Preparation: Our experts assist in compiling comprehensive technical documentation, including clinical evaluation reports, risk management files, and biocompatibility assessments.
- Clinical Evaluation and Post-Market Surveillance: We support manufacturers in conducting clinical evaluations, developing post-market surveillance plans, and preparing periodic safety update reports (PSURs).
- Authorised Representative Services: For non-EU manufacturers, our subsidiary Patient Guard Europe UG serves as a reliable Authorised Representative, ensuring continuous regulatory compliance and acting as a point of contact for EU regulators.
- QMS Implementation and ISO 13485 Compliance: We guide companies in implementing robust Quality Management Systems that align with MDR and ISO 13485 requirements, focusing on process optimization and ongoing regulatory monitoring.